Idea for this blog article: Arsha Pradhan, Student Intern (currently studying at the Asian Institute of Technology in Bangkok, Thailand).
Text of this blog article written by: Philip Button, Academy Director and Head of Research
While much emphasis, and rightly so, is given to Campylobacter jejuni, Salmonella and viruses like Norovirus as the most common cause of bacterial and viral food borne disease, we mustn’t lose sight of Listeria monocytogenes, the causal agent of listeriosis which is the most severe type of foodborne disease. Although the disease can present as a mild gastroenteritis (Riede et al., 1994), it is often more than this with neurological sequelae not common, such as life-threatening meningoencephalitis described by Büla et al. (1995). The mortality rate in vulnerable groups, such as the elderly, can approach 75% while those immunocompromised or smoking have a 50% chance of survival (Thønnings et al., 2016) It can also cause disease in animals, such as the sheep infections described by Reuter et al. (1989) in Western Australia. Other species of Listeria, apart from L. monocytogenes, have been known to cause infections in humans and animals, but these are really quite rare. L. ivanovii would be one of these other pathogenic Listeria species (Hage et al., 2014).
A wide variety of food products have been implicated in foodborne outbreaks, since this species is widespread in the natural environment. Of more concern is that L. monocytogenes has often been found in food manufacturing plants (Khan et al., 2016). In the natural environment, association with animals is common – Gray and Killinger (1966) note that 38 mammal species have been found to carry L. monocytogenes.

In recent years, 2017 and 2018, there were two significant outbreaks that should serve as a reminder about the need for vigilance with regard to L. monocytogenes. The world’s largest L. monocytogenes outbreak took place across 2017 and 2018 in South Africa. It was linked to processed meat products and ultimately resulted in 1 060 confirmed cases and 216 deaths (Tchatchouang et al., 2020). In Australia, a significant outbreak traced to rockmelons from the Riverina region of New South Wales resulted in six deaths and 18 confirmed cases – 16 in Australia and two in Singapore. Overall, L. monoytogenes is one of two key pathogens that is emerging as an important cause of foodborne disease through consumption of fresh produce (Wadamori et al., 2017).

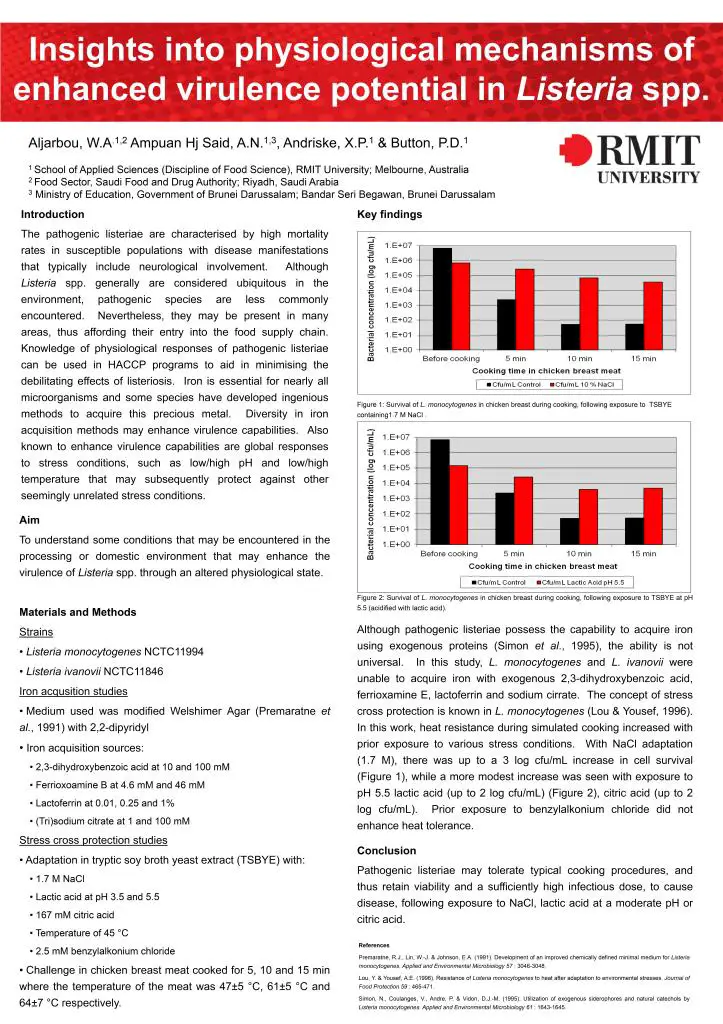
Of great significance with regard to its control is the fact that L. monocytogenes is psychrotropic. This means that if it is present in/on a food, refrigeration of that food will not have a bacteriostatic effect, in fact, it will select for its growth. The low temperatures will reduce competition in that food product, creating more favourable conditions for the growth of L. monocytogenes, due to its psychrotrophy. Furthermore, much work has demonstrated the existence of adaptive stress responses, not only to a single stress condition, such as acid (Davis et al., 1996), but that it possess a stress cross-protection system that can be initiated as a global response to different, separate stress conditions (Skandamis et al., 2008). Results from our work have also shown this – Listeria monocytogenes exposed to physiological stressors of high salt (10% NaCl) or moderately low pH in organic acid (lactic acid at pH 5.5) showed improved survival in chicken meat when cooked under normal time and temperature conditions. This really demonstrates and supports the vigilance that needs to be taken with this species, because it is very capable of survival and indeed growth under a range of conditions that normally are not tolerated by other species.
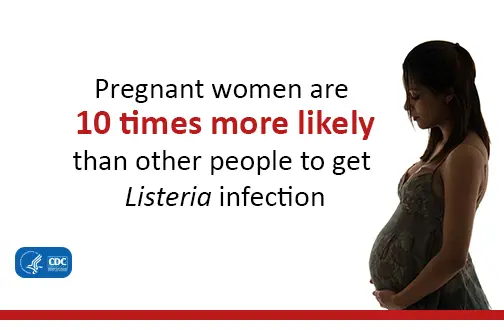
Pregnant women are often the target of awareness campaigns regarding listeriosis, although in addition, Moran et al. (2018) points out that neonates, immunocompromised people and the elderly are particularly vulnerable, and some mortality statistic were presented earlier in this article around this. However, with regard to pregnant women, this is because, in addition to gastroenteritis and a range of neurological conditions, infection by L. monocytogenes may result in various pregnancy complications, including miscarriage in the first trimester. Therefore, pregnant women are a key group that are reminded to reduce their risk by not consuming high-risk foods, such as soft cheeses.
With its significance as a foodborne pathogen, L. monocytogenes requires attention. Through good hygiene and good cleaning, GAP, GMP, a HACCP plan and the practical steps that can be taken in the home to ensure cross contamination can all help. However, remember, if it is on or in a food product you have, refrigerating that food will only make the food more hazardous from a listeriosis perspective. Therefore, as a general rule of thumb, it is always advised to reduce the time that you have food stored, anywhere. Minimise the length of time you store food in the refrigerator so as to not give psychrotropic microorganisms a chance to proliferate.
References
Büla, C. J., Bille, J., & Glauser, M. P. (1995). An epidemic of food-borne listeriosis in western Switzerland: description of 57 cases involving adults. Clinical Infectious Diseases, 20(1), 66-72.
Davis, M. J., Coote, P. J., & O’Byrne, C. P. (1996). Acid tolerance in Listeria monocytogenes: the adaptive acid tolerance response (ATR) and growth-phase-dependent acid resistance. Microbiology, 142(10), 2975-2982.
Gray, M. L., & Killinger, A. (1966). Listeria monocytogenes and listeric infections. Bacteriological reviews, 30(2), 309-382.
Hage, E., Mpamugo, O., Ohai, C., Sapkota, S., Swift, C., Wooldridge, D., & Amar, C. F. L. (2014). Identification of six L isteria species by real‐time PCR assay. Letters in applied microbiology, 58(6), 535-540.
Khan, I., Khan, J., MISKeen, S., Tango, C. N., ParK, Y. S., & Oh, D. H. (2016). Prevalence and control of Listeria monocytogenes in the food industry–a review. Czech Journal of Food Sciences, 34(6), 469-487.
Moran, L. J., Verwiel, Y., Khomami, M. B., Roseboom, T. J., & Painter, R. C. (2018). Nutrition and listeriosis during pregnancy: a systematic review. Journal of nutritional science, 7.
Reuter, R., Bowden, M., & Palmer, M. (1989). Ovine listeriosis in south coastal Western Australia. Australian veterinary journal, 66(7), 223-224.
Riedo, F. X., Pinner, R. W., Tosca, M. D. L., Cartter, M. L., Graves, L. M., Reeves, M. W., … & Broome, C. (1994). A point-source foodborne listeriosis outbreak: documented incubation period and possible mild illness. Journal of Infectious diseases, 170(3), 693-696.
Kaptchouang Tchatchouang, C. D., Fri, J., De Santi, M., Brandi, G., Schiavano, G. F., Amagliani, G., & Ateba, C. N. (2020). listeriosis outbreak in south Africa: a comparative analysis with previously reported cases worldwide. Microorganisms, 8(1), 135.
Skandamis, P. N., Yoon, Y., Stopforth, J. D., Kendall, P. A., & Sofos, J. N. (2008). Heat and acid tolerance of Listeria monocytogenes after exposure to single and multiple sublethal stresses. Food microbiology, 25(2), 294-303.
Thønnings, S., Knudsen, J. D., Schønheyder, H. C., Søgaard, M., Arpi, M., Gradel, K. O., … & Smit, J. (2016). Antibiotic treatment and mortality in patients with Listeria monocytogenes meningitis or bacteraemia. Clinical Microbiology and Infection, 22(8), 725-730.
Wadamori, Y., Gooneratne, R., & Hussain, M. A. (2017). Outbreaks and factors influencing microbiological contamination of fresh produce. Journal of the Science of Food and Agriculture, 97(5), 1396-1403.