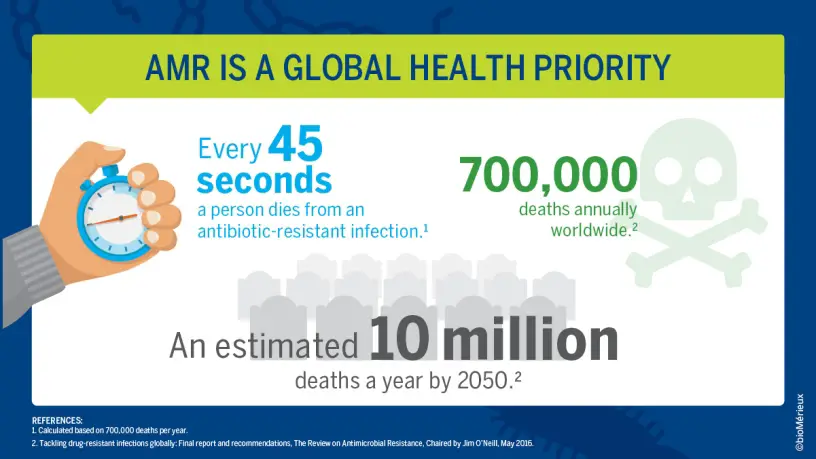
Antibiotic resistance is a significant global challenge, fast becoming one of this century’s most significant issues. Not only does it have concerns in human and veterinary medicine, in agriculture and food science, but in public health too. We must act now to stem the tide, the growing problem of antibiotic resistance, before it becomes an insurmountable obstacle and drives the demise of humanity, of civilisation.
Let us launch straight into the concerns of antibiotic use for our own personal health…
Another important problem is associated with our own microbiome, primarily our gut microbiome, since many antibiotics are taken orally. Unfortunately, a substantial number of antibiotics are prescribed rapidly and without reference to any antimicrobial sensitivity testing. Under such circumstances, patients almost demand an antibiotic prescription after visiting a clinician. The medico, under this kind of pressure from their patient, doesn’t have the time to wait up to 48 hours (or longer) for an antimicrobial sensitivity test result, typically doesn’t even request a sample, rather, prescribes a broad spectrum antibiotic, often based on nothing more than clinical observation and possible symptom history, which may be sometimes unreliable. While this is a quick and easy way to satisfy a patient, it is harmful in multiple ways. For example, indiscriminate prescription of antibiotics will contribute to the spread of antibiotic resistance genes during active infections and among human and environmental reservoirs of pathogenic bacteria. Furthermore, the patient will be unaware that taking a broad spectrum antibiotic may or may not eliminate the bacteria troubling them, but even if it does, it is highly likely to do untold damage to the host’s own flora, their microbial ecosystem. This could open the patient up to side effects or additional infections, once the protection, primarily from the gut microbiota is severely disrupted. Severely disrupted to the stage where opportunistic pathogenic bacteria could gain a ‘foothold’, resulting in an additional and subsequent infection(s). So, indiscriminate prescription of antibiotics is certainly highly likely to do more harm (in the longer term) than good (n the shorter term).

The way microorganisms can potentially address this, while largely unknown, would surely lie within the immense unknown prokaryotic diversity that remains to be discovered. A few years ago, Locey and Lennon (2016) provided an updated estimation of the total prokaryotic species on our planet, which they said, is likely to be in excess of one trillion. We currently are aware of an absolute minuscule proportion of this estimated total. Therefore, simply by intensifying research investigations of extreme environments for yet-to-be discovered microbes and developing means to actually culture them, is likely to hold a key to humanity’s success. Just through a trial and error investigation of the microbial world, we are highly likely to unlock some prokaryotic secrets that could hold value in addressing our global challenges. Really, it could very well be a numbers game – with so many undiscovered species and undiscovered potential, the answers are likely to be there, if we look long and hard enough. An important element of this though is keeping an open mind. Keeping an open mind with regard to what we are looking for, where we look for it, how we look for it, how they are cultured and more. If we don’t, we could very well miss the opportunity of a lifetime to change the course of humanity. It takes sharpness, alertness and looking at situations from a different perspective to be able to recognise potential. If Alexander Fleming hadn’t noticed on 28 September 1928 that a contaminating mould was inhibiting the growth of an important human pathogenic bacterium, the world would be a different place today. He could have easily seen the contaminating mould on that agar plate, thrown it away, and an opportunity to change the course of humanity would have been lost.
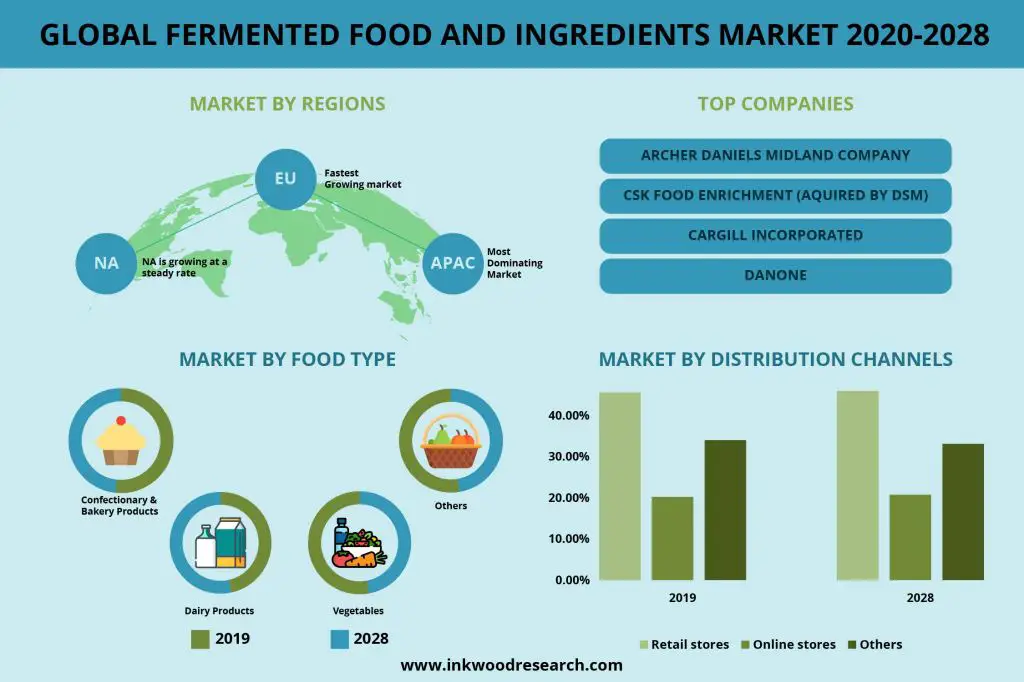
Scouring the unexplored microbial world for compounds of potential use which can be used to address human challenges is one aspect, and a key area where global efforts should be directed. However, as old as fermented foods and probiotics are, they hold much potential to further address issues of public health associated with diet, which really, is the cornerstone to good health of everyone. Even though each of us contain untold diversity in our own microbiome, it is still not well understood. Innovative analytical methods are needed to improve characterisation of the human microbiome. Furthermore, the way it is linked to a range of elements and indicators of health needs to be elucidated. This could result in targeted food product development activities and direct public health messages, based on sound science, around what will be beneficial for health within the context of today’s lifestyle. Furthermore, fermented foods are trending and this trend and positive image by consumers should be explored further to produce diverse fermented foods that are able to bring great public health benefits while satisfying people’s increasing desire for exotic tastes with new foods. There are countless microorganisms of fermentative potential, and numerous types of food substrates that could be used to develop a wide range of natural and healthy foods. Consumers’ positivity towards fermented foods and beverages should really be explored further to bring them products likely to gain rapid market acceptance. The idea is that with improved public health from improved personal health resulting from healthier eating of diverse food products of microbial origin, there would be less reliance on antibiotics.