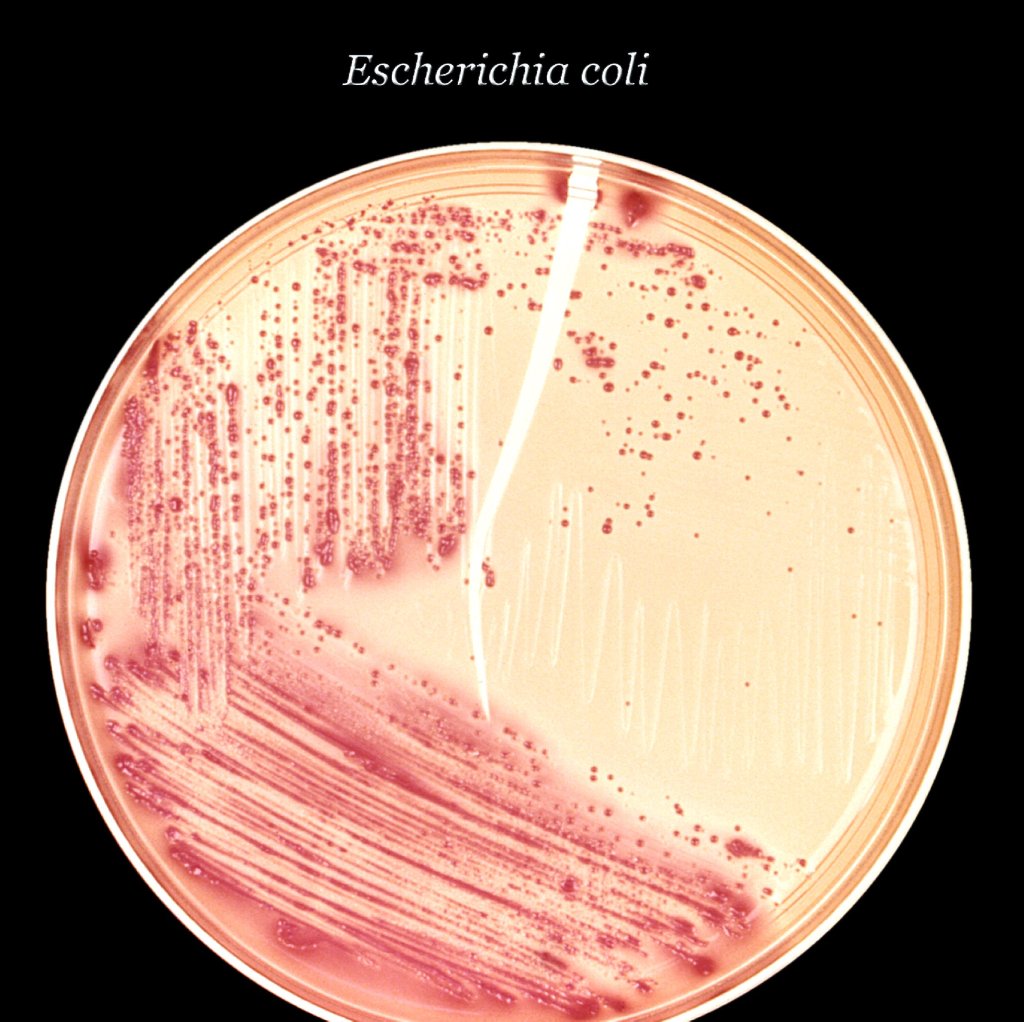
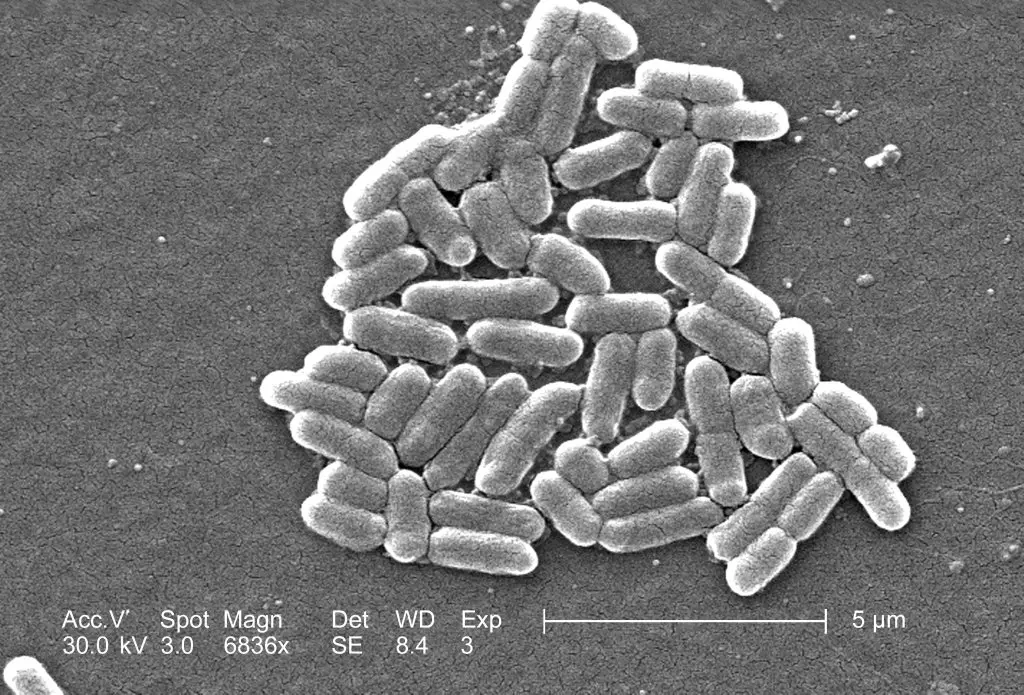
Pathogenic Escherichia coli (E. coli) are classified into several categories based on the virulence factors they possess. Some of the most common types are:
- Enterotoxigenic E. coli (ETEC) – Causes diarrhea in travelers and in developing countries.
- Enteropathogenic E. coli (EPEC) – Causes diarrhea, especially in young children.
- Enteroaggregative E. coli (EAEC) – Also causes diarrhea, often associated with malnutrition and poor hygiene.
- Shiga toxin-producing E. coli (STEC) – Causes severe foodborne illness, including Hemorrhagic Colitis (HC) and Hemolytic Uremic Syndrome (HUS).
- Extraintestinal pathogenic E. coli (ExPEC) – Causes urinary tract infections, sepsis, and other infections outside the gut.
It is important to note that not all strains of E. coli are pathogenic, and many are even beneficial to the human gut.
Enterotoxigenic Escherichia coli (ETEC) – Produce and secrete one or more enterotoxins that disrupt the normal function of the gut and cause watery diarrhea. The enterotoxins produced by ETEC are called heat-labile toxin (LT) and heat-stable toxin (ST), which mimic the action of the human gut hormones and stimulate fluid secretion, leading to diarrhea.
LT targets the small intestine and stimulates excessive secretion of chloride ions into the lumen of the gut, causing osmotic diarrhea. ST targets the large intestine and stimulates the production of prostaglandins, leading to increased secretion of fluid and electrolytes into the gut lumen.
In addition to the enterotoxins, ETEC can also attach to the surface of the gut epithelium and interfere with the normal function of the gut, causing inflammation and damage to the gut lining. This can lead to decreased nutrient absorption and dehydration, which can become life-threatening in severe cases, especially in young children, elderly individuals, and those with weakened immune systems.

Enteropathogenic Escherichia coli (EPEC) – Attach to the intestinal epithelium and induce changes in the host cell cytoskeleton, leading to the formation of a characteristic lesion known as “attaching and effacing (A/E) lesion.”
The attachment of EPEC to the gut epithelium is facilitated by a type of adhesion molecule known as “bundle-forming pilus” (BFP). This allows the bacteria to form a close association with the host cells and secrete effector proteins that alter the cytoskeleton and disrupt the normal function of the gut.
The alterations in the host cell cytoskeleton caused by EPEC result in the characteristic A/E lesion, which leads to the detachment of the bacteria from the gut epithelium and their release into the gut lumen, allowing them to spread to other parts of the gut and cause further damage.
The A/E lesion and the release of bacterial products into the gut can also stimulate an immune response and cause inflammation, leading to diarrhea and other symptoms of disease. EPEC infection is most commonly seen in young children, but can also occur in adults, particularly in developing countries where hygiene and sanitation conditions may be poor.
Enteroaggregative Escherichia coli (EAEC) – Form biofilm-like aggregates on the gut epithelium, which can cause chronic diarrhea, abdominal pain, and malnutrition.
EAEC are able to attach to the gut epithelium and form large clusters, which can cause the gut to become inflamed and result in the release of pro-inflammatory cytokines and other toxic substances. The aggregates can also interfere with the normal functioning of the gut, leading to decreased nutrient absorption and fluid secretion, leading to diarrhea.
In addition to the aggregates, EAEC can also produce a range of virulence factors, including cytotoxins, hemolysins, and adhesins, which can further damage the gut and contribute to the symptoms of disease.
EAEC infections are most commonly seen in young children, particularly in developing countries where hygiene and sanitation conditions may be poor. They can also occur in adults, especially in individuals with weakened immune systems or who have recently traveled to areas with poor hygiene and sanitation.
Shiga toxin-producing Escherichia coli (STEC) – Produce and secrete Shiga toxins, which can damage the gut and cause severe foodborne illness, including Hemorrhagic Colitis (HC) and Hemolytic Uremic Syndrome (HUS).
STEC produce two types of Shiga toxins, called Stx1 and Stx2, which are toxic to human cells and can cause extensive damage to the gut, leading to diarrhea and other symptoms of HC. The toxins can also enter the bloodstream and cause damage to other organs, leading to HUS, a serious and potentially life-threatening complication.
HUS is characterized by the formation of small blood clots in the small blood vessels of the body, which can lead to reduced blood flow and damage to organs, including the kidney, brain, and heart. HUS can cause a range of symptoms, including decreased urine output, abdominal pain, and in severe cases, seizures and coma.
STEC infections are typically contracted through the consumption of contaminated food, including undercooked meat, raw milk, and contaminated fruits and vegetables. They can also be spread through person-to-person contact, particularly in outbreaks linked to food preparation and handling.
Extraintestinal pathogenic Escherichia coli (ExPEC) – These E. coli cause disease outside of the gastrointestinal tract, in other parts of the body such as the urinary tract, bloodstream, and other organs. They are typically responsible for a range of infections, including urinary tract infections (UTIs), sepsis, and meningitis.
ExPEC are able to cause disease by producing a range of virulence factors, including adhesins, fimbriae, toxins, and enzymes, which allow the bacteria to colonize and infect various tissues in the body. The virulence factors produced by ExPEC can also contribute to the pathogenesis of disease by causing inflammation, damaging host cells, and disrupting normal host processes.
UTIs are the most common type of infection caused by ExPEC, and are characterized by symptoms such as painful urination, cloudy urine, and lower abdominal pain. ExPEC can also cause sepsis, a severe and potentially life-threatening systemic infection, and meningitis, an inflammation of the protective membranes that surround the brain and spinal cord.
ExPEC infections are typically acquired through the spread of bacteria from the gut to other parts of the body, or through the introduction of bacteria into the body through a break in the skin or a medical procedure. They can also be spread through person-to-person contact, particularly in outbreaks linked to health care facilities.